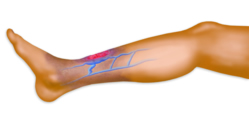
 Other types of venous disease include: Chronic Vein Insufficiency (CVI), Superficial Vein Thrombophlebitis, Deep Vein Thrombosis, Venous Ulcers and Chronic Edema. These conditions are the result of elevated pressure in the veins in the legs caused by leakage of the vein valves. The elevated pressure damages the veins and skin of the legs.
Other types of venous disease include: Chronic Vein Insufficiency (CVI), Superficial Vein Thrombophlebitis, Deep Vein Thrombosis, Venous Ulcers and Chronic Edema. These conditions are the result of elevated pressure in the veins in the legs caused by leakage of the vein valves. The elevated pressure damages the veins and skin of the legs.
Illustration: Example of venous ulcer and associated symptoms of redness and swelling.
FAQs About Varicose and Spider Veins
This information is derived and reproduced in part from American Heart Lung and Blood Institute, and WomensHealth.Gov
Varicose (VAR-i-kos) veins are enlarged veins that can be blue, red, or flesh-colored. They often look like cords and appear twisted and bulging. They can be swollen and raised above the surface of the skin. Varicose veins are often found on the thighs, backs of the calves, or the inside of the leg. During pregnancy, varicose veins can form around the vagina and buttocks.
Spider veins are like varicose veins but smaller. They also are closer to the surface of the skin than varicose veins. Often, they are red or blue. They can look like tree branches or spiderwebs with their short, jagged lines. They can be found on the legs and face and can cover either a very small or very large area of skin.
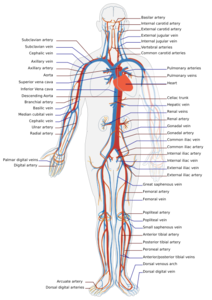
Varicose veins are caused by weakening of the vein walls resulting in enlargement of the vein and leaking of the vein valves. The heart pumps blood filled with oxygen and nutrients to the whole body through the arteries. Veins then carry the blood from the body back to the heart. As your calf muscles squeeze, they push blood back to the heart from your lower body against the flow of gravity. Veins have valves that act as one-way flaps to prevent blood from flowing backwards as it moves up your legs. If the valves leak, blood can flow backwards within the veins and collect in the legs. (This problem is called venous insufficiency.) Backed-up blood increases the pressure in the vein which causes them to enlarge and become varicose.
Spider veins can be caused by the backup of blood. They can also be caused by hormone changes, exposure to the sun, and injuries.
About 50 to 55 percent of women and 40 to 45 percent of men in the United States suffer from some type of vein problem. Varicose veins affect half of people 50 years and older.
Many factors increase a person's chances of developing varicose or spider veins. These include:
Increasing age: As you get older, the vein walls become less elastic and may weaken causing enlargement.
Medical history: Having family members with vein problems also increases your risk. About half of all people who have varicose veins have a family member who has them too.
Hormonal changes: These occur during puberty, pregnancy, and menopause. Taking birth control pills and other medicines containing estrogen and progesterone also may contribute to the forming of varicose or spider veins.
Pregnancy: During pregnancy, there is a huge increase in the amount of blood in the body. This can cause veins to enlarge. The growing uterus also puts pressure on the veins. Varicose veins usually improve within 3 months after delivery. More varicose veins and spider veins usually appear with each additional pregnancy.
Obesity: Being overweight or obese can put extra pressure on your veins. This can lead to varicose veins.
Lack of movement: Sitting or standing for a long time increases the pressure inside the veins and may force your veins to work harder to pump blood to your heart. This may be a bigger problem if you sit with your legs bent or crossed.
Sun exposure: This can cause spider veins on the cheeks or nose of a fair-skinned person.
Most varicose and spider veins appear in the legs due to the pressure in the veins, force of gravity, and task of carrying blood from the bottom of the body up to the heart. Compared with other veins in the body, leg veins have the toughest job of carrying blood back to the heart. They endure the most pressure. This pressure can be higher than the strength of the walls of the veins.
Varicose veins can often be seen on the skin. Some other common symptoms of varicose veins in the legs include:
Aching pain that may get worse after sitting or standing for a long time
Throbbing or cramping
Heaviness
Swelling
Rash that’s itchy or irritated
Darkening of the skin (in severe cases)
Restless legs
Spider veins rarely are a serious health problem, but they can cause uncomfortable feelings in the legs. If there are symptoms from spider veins, most often they will be itching or burning. Less often, spider veins can be a sign of blood backup deeper inside that you can’t see on the skin. If so, you could have the same symptoms you would have with varicose veins.
Varicose veins may not cause any problems, or they may cause aching pain, throbbing, and discomfort. In some cases, varicose veins can lead to more serious health problems. These include:
* Sores or skin ulcers due to chronic (long-term) backing up of blood. These sores or ulcers are painful and hard to heal. Sometimes they cannot heal until the backward blood flow in the vein is repaired.
* Bleeding. The skin over the veins becomes thin and easily injured. When an injury occurs, there can be significant blood loss.
* Superficial thrombophlebitis (throm-bo-fli-BYT-uhs), which is a blood clot that forms in a vein just below the skin. Symptoms include skin redness; a firm, tender, warm vein; and sometimes pain and swelling.
* Deep vein thrombosis, which is a blood clot in a deeper vein. It can cause a “pulling” feeling in the calf, pain, warmth, redness, and swelling. However, sometimes it causes no significant symptoms. If the blood clot travels to the lungs, it can be fatal.
You should see a doctor about varicose veins if:
* The vein has become swollen, red, or very tender or warm to the touch
* There are sores or a rash on the leg or near the ankle
* The skin on the ankle and calf becomes thick and changes color
* One of the varicose veins begins to bleed
* Your leg symptoms are interfering with daily activities
* The appearance of the veins is causing you distress
If you’re having pain, even if it’s just a dull ache, don’t hesitate to get help.
Varicose veins are treated with lifestyle changes and medical treatments. These can:
* Relieve symptoms
* Prevent complications
* Improve appearance
Your doctor may recommend lifestyle changes if your varicose veins don’t cause many symptoms.
If symptoms are more severe, your doctor may recommend medical treatments. Some treatment options include:
Compression Stockings: Compression stockings put helpful pressure on your veins. There are 3 kinds of compression stockings:
* Support pantyhose, which offer the least amount of pressure. These also often are not “gradient” or “graduated.” That means they provide pressure all over instead of where it is needed most.
* Over-the-counter gradient compression hose, which give a little more pressure. They are sold in medical supply and drugstores.
* Prescription-strength gradient compression hose, which offer the greatest amount of pressure. They are sold in medical supply and drugstores. You need to be fitted for them by someone who has been trained to do this.
Sclerotherapy
(SKLER-o-ther-a-pee): Sclerotherapy is the most common treatment for spider veins. The doctor uses a needle to inject a liquid chemical into the vein. The chemical injures the lining of the vein walls causing them to stick together, and seal shut. This stops the flow of blood, and the vein turns into scar tissue. In a few weeks, the vein should fade. This treatment does not require anesthesia and can be done in your doctor's office. You can return to normal activity right after treatment.
The same vein may need to be treated more than once. Treatments are usually done every 4 to 6 weeks. You may be asked to wear gradient compression stockings after sclerotherapy to help with healing and decrease swelling. This treatment is very effective when done correctly.
Possible side effects include:
* Stinging, red and raised patches of skin, or bruises where the injection was made. These usually go away shortly after treatment.
* Spots, brown lines, or groups of fine red blood vessels around the treated vein. These also usually go away shortly after treatment.
* Lumps of blood that get trapped in vein and cause inflammation. This is not dangerous. You can relieve swelling by applying heat and taking aspirin. Your doctor can drain the trapped blood with a small pinprick at a follow-up visit.
There is a type of sclerotherapy called ultrasound-guided sclerotherapy (or echo-sclerotherapy). This type of sclerotherapy uses ultrasound imaging to guide the needle. It is useful in treating larger veins that cannot be seen on the skin’s surface. It may be used after surgery or endovenous techniques if the varicose veins return. This procedure can be done in a doctor’s office. Possible side effects include skin sores, swelling, injection into an artery by mistake, or deep vein thrombosis (a potentially dangerous blood clot).
Surface Laser Treatments: In some cases, laser treatments can effectively treat spider veins and smaller varicose veins. This technique sends very strong bursts of light through the skin onto the vein. This makes the vein slowly fade and disappear. Not all skin types and colors can be safely treated with lasers.
No needles or incisions are used, but the heat from the laser can be quite painful. Cooling helps reduce the pain. Laser treatments last for 15 to 20 minutes. Generally, 2 to 5 treatments are needed to remove spider veins in the legs. Laser therapy usually isn’t effective for varicose veins larger than 3 mm (about a tenth of an inch). You can return to normal activity right after treatment.
Possible side effects of lasers include:
* Redness or swelling of the skin right after the treatment that disappears within a few days
* Discolored skin that will disappear within 1 to 2 months
* Burns and scars from poorly performed laser surgery, though this is rare
Endovenous Techniques (Radiofrequency and Laser): These methods for treating the deeper veins of the legs, called the saphenous (SAF-uh-nuhs) veins, have replaced surgery for most patients with severe varicose veins. These techniques can be done in a doctor’s office. The doctor puts a very small tube, called a catheter, into the vein. A small probe is placed through the tube. A device at the tip of the probe heats up the inside of the vein and closes it off. The device can use radiofrequency or laser energy to seal the vein. The procedure can be done using just local anesthesia. You might have slight bruising after treatment. Healthy veins around the closed vein take over the normal flow of blood. The symptoms from the varicose vein improve. Usually, veins on the surface of the skin that are connected to the treated varicose vein will also shrink after treatment. If they don’t, these connected veins can be treated with sclerotherapy or other techniques.
Endovenous Techniques-Medical Adhesive (VenaSeal Closure): This method is used for treating the deeper veins of the legs, called the saphenous (SAF-uh-nuhs) veins. It has been in use in the U.S. since 2015, and it can be done in a doctor’s office. The doctor puts a very small tube, called a catheter, into the vein. A small probe is placed through the tube. The catheter deliver small amounts of medical adhesive into the diseased vein. The vein is then closed off. The device can use radiofrequency or laser energy to seal the vein. The procedure can be done using local anesthesia and in just a single location. You might have slight bruising after treatment. Healthy veins around the closed vein take over the normal flow of blood. The symptoms from the varicose vein improve. Usually, veins on the surface of the skin that are connected to the treated varicose vein will also shrink after treatment. If they don’t, these connected veins can be treated with sclerotherapy or other techniques. Typically, patient can return to normal activity immediately following the procedure and are not required to wear post-procedure compression hose.
Surgery: Surgery is used mostly to treat very large varicose veins. Types of surgery for varicose veins include:
* Microphlebectomy (also called "Ambulatory Phlebectomy"): With microphlebectomy, tiny cuts are made in the skin, and hooks are used to pull the vein out of the leg. Only the parts of your leg that are being pricked will be numbed with anesthesia. The vein is usually removed in 1 treatment. Very large varicose veins can be removed with this treatment while leaving only very small scars. Removing the veins does not affect the circulation of blood in the leg. Veins deeper in the leg take care of the larger volumes of blood. Patients can return to normal activity the day after treatment. Possible side effects of the treatment include slight bruising and temporary numbness. Microphlebectomy is normally done on an outpatient basis.
* Surgical Ligation and Stripping. Surgical ligation and stripping are rarely used in the present, because they have been replaced with less invasive therapies. With this treatment, problem veins are tied shut and completely removed from the leg through large cuts in the skin. This surgery requires general anesthesia and must be done in an operating room. It takes between 1 and 4 weeks to recover from the surgery.
Not all varicose and spider veins can be prevented. But, there are some steps you can take to reduce your chances of getting new varicose and spider veins. These same things can help ease discomfort from the ones you already have:
* Wear sunscreen to protect your skin from the sun and to limit spider veins on the face.
* Exercise regularly to improve your leg strength, circulation, and vein strength. Focus on exercises that work your legs, such as walking or running.
* Control your weight to avoid placing too much pressure on your legs.
* Don’t cross your legs for long times when sitting. It’s possible to injure your legs that way, and even a minor injury can increase the risk of varicose veins.
* Elevate your legs when resting as much as possible.
* Don’t stand or sit for long periods of time. If you must stand for a long time, shift your weight from one leg to the other every few minutes. If you must sit for long periods of time, stand up and move around or take a short walk every 30 minutes.
* Wear elastic support stockings and avoid tight clothing that constricts your waist, groin, or legs.
* Avoid wearing high heels for long periods of time. Lower-heeled shoes can help tone your calf muscles to help blood move through your veins.
* Eat a low-salt diet rich in high-fiber foods. Eating fiber reduces the chances of constipation, which can contribute to varicose veins. High-fiber foods include fresh fruits and vegetables and whole grains, like bran. Eating less salt can help with the swelling that comes with varicose veins.
Current treatments for varicose veins and spider veins have very high success rates compared to traditional surgical treatments. Over a period of years, however, more abnormal veins can develop because there is no cure for chronic venous insufficiency. Ultrasound can be used to keep track of how badly the valves are leaking (venous insufficiency). Ongoing treatment can help keep this problem under control. The single most important thing you can do to slow down the development of new varicose veins is to wear gradient compression support stockings as much as possible during the day
Link Library
This panel includes outbound links to trusted sources of medical information such as the National Health Library, Medline and American Heart Lung and Blood Institute. Links will direct you to a new browser window. Please note that all information contained at these web sites is meant for informational purposes only, and is not intended as a substitute for an actual physician visit.
National Health Library | American Heart Lung and Blood Institute - Overview, FAQs and more
http://www.nhlbi.nih.gov/health/dci/Diseases/vv/vv_all.html
National Health Library | Medline Plus
Varicose Vein Introduction and Associated Links